Friday, November 6, 2009
EYE EXAM
-name
-CC
LOOK
-look at good eye 1st
-wash hands
FEEL
-bony prominences
-upper eyelid(jaundice) and lower eyelid(anemia)
TEST
1.Snellen (20ft/6m away)
2.Ishihara (arms length)
3.visual field
4.Blind spot
5.Accomodation
6.Pupillary light reflex
7.Ophtalmoscope
bye bye.
Upper Limb MSK
2) Ask for Name
3) Privacy confidentality and Consent
4) Explain to patient the need for exposure, allow to stop if pain , and wash hands
5)Inspection!
Look for Sweats Signs + compare ( give a open commentary)
6) FEEL!
Jugular notch--->clavicle----> acromion---> superior border----> spine----> lateral border---> inferior angle---> medial border
coracoid process---> bicipital tendon--tenderness (ask patient to flex if you want)
7) MOVE!!
Place hand on acromio-clavicular joint when moving arm--> check for crepitus
ACTIVE FIRST, then passive
Flexion, extension
Abduction, adduction
Internal and external rotation
8) Painful arc syndrome - 60 degress to 120 degrees
Lower Limb MSK Examination
2) Ask patient's name & age
3) Short history- when and why?
4) Explain to patient about the examination about exposure
5) PLEASE TELL ME IF YOU FEEL ANY PAIN/ PLEASE STOP ME IF THERE IS ANY PAIN
6) WASH YOUR FREAKING HANDS
7) LOOK!!!!
SWEATS, Compare both sides
8) FEEL!!!
ASIS, pubic tubercle, (femoral pulse in between),
greater trochanter of femur,
tibial Tuberosity,
Feel for Baker's cyst
condyles,
patella, ( patella Tap, Bulge test-milk test)
medial and lateral malleolus
9)Movement (Active first , then passive)
Hip - Flexion/Extension , Abduction/Adduction, Internal/External R.
Knee - Flexion/Extension ,
Ankle - Plantarflex, Dorsiflex ; Eversion/Inversion
Specific Test
1) Tredenlenburg (double check this *)
2) Thomas Test *
3) Drawers Test
4) Lachman Test - ACL
5) Mcmurray Test - Medial Meniscus and Lateral Meniscus
6) Patella Apprehension *(during palpation)- move patella laterally, and extend your knee.
7) Bulge Test * (during palpation)- Milking
8) Semen Test - Squeeze your Calve muscles, if normal got plantarflexion
Measurement
1) True Length - asis to the medial malleolus
2) Apparent Length- belly button to medial malleolus
Thursday, November 5, 2009
Back Examination
2) Ask patient's name & age
3) Short history- when and why?
4) Explain to patient that the exam requires him to remove shirt
5) Ask patient to remove shirt while YOU WASH YOUR FREAKING HANDS
6) LOOK!!! - curvatures, SWEATS, fasciculations
7) FEEL!!!-
Protuberance, C2, C7, C6, T1 ,
spine of scapula----> sup. T2, inf. T7,
Illiac crest- L4,L5
Spinous process + Transverse process
Erector Spinae muscles0- wasting? fasciculations?
8) Measure lumbar extension- locate L5, 10cm up, 5 cm down----> more than 4cm= normal
9) MOVE!!!
Neck- flexion, extension, lateral rotation, lateral flexion
Thoracic- Rotation
Lumbar- flexion, extension, lateral flexion
10) Specific Tests
SLR----> BARRRHHH GADD's test (dorsiflex), LARRR SARGGHH's test (flex hip, extend leg)
11) Say your farewells to the patient, and thank patient.
History Taking!!!!!
HPI
Systems Review
PMH
Past Surgical Hx
Obs & Gyn
Drugs & Medication
Allergy
Smoking & Alcohol
Fam Hx
Social Hx
Occupational & Travel Hx
Sexual Hx
OSCE BABY
Thursday, October 22, 2009
SPina BIfida (Bowel,bladder control, sensation,dermatome)
Bladder and bowel problems in spina bifida
1. A person with spina bifida is usually born with an undamaged urinary system. Over time, paralysis leads to neurogenic bladder. It is caused by damage to the nerves in the sacral area:
- The bladder
- The urinary sphincter
- The muscular flap attached to the ureter.
2. Can be either flaccid or spastic:
- Flaccid - limp and cannot contract completely to force urine out. When the flaccid bladder becomes full, excess urine spills over and flows out of the body through the urethra. Urine dribbles out continually and when excess pressure is put on the bladder (laughing or crying), this dribbling becomes more severe. However, the bladder never empties completely and some (residual) urine always remains.
- Spastic - Does not store urine at all. The muscles that line this type of bladder are extremely sensitive and irritable. They contract and expel urine immediately after it enters the bladder.
3. Damage to the sphincter muscle can be either too tight or too loose. When the sphincter muscle is tight, urine becomes trapped in the bladder and is often forced back up the ureters to the kidney. If the sphincter muscle is too loose, however, urine continually leaks out of the body.
4. This backward flow of urine can be very damaging to the urinary system and especially the kidneys. Normally, a muscular flap on the ureters closes and once the urine flows out of the kidneys, it cannot flow back. However, the muscles that control this flap are often damaged and instead of following the path from the kidneys to the bladder and outside of the body, the urine flows back up the ureters to the kidney.
5. Urine infection - A person with spina bifida who has paralysis in the lower extremities should monitor the appearance of their urine carefully since they may not be able to feel the first warning signs — pain while urinating, for example — of a urinary tract infection.
Lack of sensation
For lower lesions, it is not so straightforward. Children who are able to walk fairly well seem only to lack some movement in the feet, but loss of sensation will usually be in some areas of the feet, right up the leg, and also the buttocks.
1. Possible problems
a. Burns
- Sunburn on legs and feet (especially if shoes and socks are usually worn).
- Wheelchair left in hot sun. The child transferring back into a hot wheelchair may burn buttocks, legs and feet.
- Hot drinks/chips held on lap.
- Hot car/bus seat.
b. Scrapes (Child crawling on rough ground (especially pool surrounds) may scrape knees, ankles and toes)
c. Pressure - Pressure areas are red areas of skin caused by prolonged pressure on one area. Any red area that disappears within 30 minutes is no problem, but one which persists from day to day needs attention. Pressure areas can develop into very nasty sores if they are not treated early and effectively. They can in some cases take months or years to heal.
Gait
General gait features include overall limb hypotonicity, flexed posturing of the lower limbs, decreased velocity in an attempt to conserve energy and significant foot deformities.
Possible OSCE Station- HEP/ Lifestyle Station
The following is the stem we were given for our end of year OSCE last year -
You are a doctor in a GP clinic. Arif Asri, a 36-year-old sales manager, has come to your clinic because he is very concerned about his health and wants to know what he can do to improve it. He has recently been diagnosed as having diabetes mellitus. Apart from this, he has gained a lot of weight in the past two years, and also smokes about 20 cigarettes a day. On examination his BP is 130/90 mm Hg and his BMI is 30.
Tasks:
You are required to:
a) Take a brief history of his lifestyle based on the ESSENCE model (4 mins.)
b) Suggest a plan for changing any one aspect of his lifestyle (diet, exercise, or smoking), using a behaviour change strategy e.g. Prochaska Diclemente cycle of behaviour change, and a model for target setting (4 mins).
Approaching this Station -
- Introduce yourself, consent, explain what you'll be doing -
'Hi, my name is ______, how are you? I understand that you've come in today because you're concerned about your health?'
- Much of the information you would normally gain from a history has been provided in the stem, so don't spend too much time going over it – remember you only have 8 minutes (sounds like ages – it's not always!)
- “So you're looking at improving your health, and that's fantastic. Acknowledging that you want to change is the first step so it's great that you've come in to see me.” Positive reinforcement is always useful and very helpful in developing rapport.
- “Before we start discussing the changes that we would like to implement, first I'd like to find out a bit more about your current lifestyle – so tell me, are you getting much exercise at the moment?
- Then just move systematically through the ESSENCE model – or whichever plan works best for you. Personally I find that starting with Exercise is a good question to start off with as people will expect it and (initially at least – while you're still developing rapport) it's easier to answer than “where do you get a sense of meaning from.
- So, working through the acronym, just have a general question in mind for each aspect -
E – Education – 'what do you know about how your habits affect your health?'
S – Stress Management – 'do you ever feel stressed about work/relationships? How do you deal with this?'
S – Spirituality – 'do you get a sense of meaning from somewhere in particular? Do you attend church?'
E – Exercise – 'what sort of exercise do you do? How much would you do in a week?'
N – Nutrition – 'what would you eat for each meal in an average day?'
C – Connectedness – 'do you feel close to your friends or family? How much time do you spend with them/how often do you see them?'
E - Environment – 'who are you living with? Are you happy living with them? Do you think they would support your new lifestyle changes?'
- And then, using BASK or Prochaska DiClemente, set up a plan for the patient to begin these lifestyle changes. Personally I find smoking to be the easiest as there is generally just the one aspect – needing to cut down as much as possible. Nutrition and Exercise are both good ones to look at though (remembering that this stem has only asked you to look at one.)
BASK model for behavior change
Behaviors
Attitudes
Skills
Knowledge
SAME model for goal setting
Specific
Attainable
Measurable
Enjoyable
Prochaska DiClemente Cycle for change
Precontemplation
Contemplation
Preparation
Action
Maintenance
Relapse (relapse is not failure)
8. For this I would probably talk to patient through Prochaska (I find it easy to explain) – although stick with whichever you are most comfortable/familiar with.
Eg - “Are you familiar with the Prochaska DiClemente cycle? It's a system that is used for helping people initiate behaviour change. Most importantly, we need to identify the stage as which you are at. The first stage is Precontemplation, but by coming in to see me I recognise that you have already begun thinking about the changes we need to make. The next stage is contemplation, and this is where you begin to weigh up the benefits of embracing a healthier lifestyle, and it's great to see that you've done that. The next phase is Preparation, and this is what I'd like to work with you to do today... Proper preparation is very important etc... You've mentioned that you'd like to cut down on smoking -
- reduce number of cigarettes
- have you ever heard of nicotine patches?
- reward yourself when you resist a cigarette
- remove yourself from/reduce the number of situations where you want to smoke – high stress, 'smoko' at work etc
When you leave today I'd like you to begin to put this into Action... After this it is important to Maintain these changes... if you do move into Relapse, where the lifestyle changes we discuss are not upheld, remember that this is not a 'failure' as such... You can try again etc...
Hydrocephalus
Sign and symptoms
-Symptoms of hydrocephalus vary with age, disease progression, and individual differences in tolerance to the condition. For example, an infant's ability to compensate for increased CSF pressure and enlargement of the ventricles differs from an adult's. The infant skull can expand to accommodate the buildup of CSF because the sutures (the fibrous joints that connect the bones of the skull) have not yet closed.
Symptoms in infants
* Poor feeding
* Irritability
* Reduced activity
* Vomiting
Symptoms in children
* Slowing of mental capacity
* Headaches (initially in the morning) that are more significant than in infants
because of skull rigidity
* Neck pain suggesting tonsillar herniation
* Vomiting, more significant in the morning
* Blurred vision: This is a consequence of papilledema(optic disc swelling that
is caused by increased intracranial pressure. ) and later of optic atrophy
* Double vision: This is related to unilateral or bilateral sixth nerve palsy
* Stunted growth and sexual maturation from third ventricle dilatation: This can lead to obesity and to precocious puberty or delayed onset of puberty.
* Difficulty in walking secondary to spasticity: This affects the lower
limbs preferentially because the periventricular pyramidal tract is stretched
by the hydrocephalus.
* Drowsiness
Sore Foot Infection
Occurs when there is pressure on the feet followed by contamination by foreign materials or colonization by bacteria. Normally, this restricts flow of blood, oxygen, and nutrients to the area. Subsequently the skin cells die. A person with spina bifida has areas of skin which do not have any feeling and often have partial or complete paralysis, and so does not receive these messages. If the pressure continues the blood supply is cut off, causing pressure sores.
Prevention
-Regular Visual Checks
-Suitable wheelchairs, footwear, and braces must be fitted.
-Wearing loose clothing can help prevent rubbing. Tight clothing can reduce circulation
-Ensuring the skin is kept clean and dry will help protect from rashes and bacteria.
-Exercising regularly may improve circulation considerably lessening the risk of pressure sores.
Grade
Grade 1 – skin discolouration, usually red, blue, purple or black.
Grade 2 – some skin loss or damage involving the top-most skin layers.
Grade 3 – necrosis (death) or damage to the skin patch, limited to the skin layers.
Grade 4 – necrosis (death) or damage to the skin patch and underlying structures, such as tendon, joint or bone
Treatment
Grade 1 and 2 only need pressure relieve and daily check up of the foot. if there is any open wound, clean and dressing to avoid infection. The goals are to provide a moist wound environment, encourage drainage, avoid build-up of necrotic tissue, and keep the bacterial count low.
For infection, the most frequently used medications for foot infections are first-generation cephalosporins, clindamycin (for patients allergic to penicillin), amoxicillin, clavulanate (Augmentin), and levofloxacin (Levaquin) and are directed toward the most common organisms, including S aureus, S epidermidis, and Streptococcus species.
Severe limb-threatening foot infections require aggressive treatment with a combination of local wound care, intravenous antibiotics, and surgical debridement. Infections with open wounds, usually are inoculated with a combination of gram-positive and gram-negative aerobes and anaerobes. These should be treated with broad-spectrum antimicrobials such as ampicillin and sulbactam (Unasyn), ticarcillin and clavulanate (Timentin), or piperacillin and tazobactam (Zosyn) In the patient who is allergic to penicillin, intravenous clindamycin in combination with oral ciprofloxacin, levofloxacin, or gatifloxacin may be used.Wounds that are suspected of containing very aggressive gram-negative organisms should be covered additionally with an aminoglycoside.
Wednesday, October 21, 2009
Tuesday, October 20, 2009
social relationship problems faced by spina bifida children
Personal-social skills- reflection, self-knowledge, rules, control of impluses, conscience
Cognitive- problem solving, multistep procedures
Social acceptance- by the age of 12, the search for friendship and popularity and avoiding humiliation may exceed pleasing parents and getting good grades.
Transitions between primary school and secondary school. May not understand that relationship requires discretion and careful pacing, and not make inappropriate gestures or action too early. Do not know how to interact with other children in different settings like bus stop, cafeteria, gymnasium.
4 types of children- generally depends on social skills:
- popular- sought after, looked-up to, respected by peers- know how to deal with different situation and have manipulation skills
- controversial- highly liked and disliked
- neglected- unnoticed
- rejected- ostracized/ stay away from
May encounter social isolation due to lack of social skills
Monday, October 19, 2009
Clinical Skill Revision, Take 1
http://www.resus.org.au/arc_guideline_changes.pdf
DR ABC
Danger
Response
Airway
Breathing
Circulation

Carotid
Brachial
Radial
Femoral
Popliteal
Dorsalis pedis
Posterior tibial
Blood pressure - important points!!
- Exercise, coffee?? if yes, wait 5 mins
- cross leg? UNCROSS LEG!!
1. Introduction & ASK PATIENT'S NAME
Hello, my name is Tom Cruise, and I am a first year medical student.
2.Purpose
I'm here as instructed by my doctor to take your blood pressure.
3. Explaination & Consent
This procedure will require me to put this band/cuff around your arm and I will inflate the cuff/band. This may be a bit uncomfortable but I can stop if it's too uncomfortable. Is that okay with you?
4. ASK FOR P&C and not Phey Chien-
WASH HANDS!!
ASK PATIENT IF HE/SHE HAS TAKEN COFFEE/ HAD SMOKE/ EXERCISE before coming - WAIT FOR 5 MINUTES
ASK PATIENT NOT TO CROSS LEGS
5. Remove air from cuff.
6. Palpate for patient's brachial artery and put cuff around patient's arm.
7. Palpate for radial pulse and inflate arm cuff.
8. Feel radial pulse until it disappears. This is the estimated systolic pressure.
9. Deflate arm cuff.
10. Tap on diaphragm to check stethoscope and then place stethoscope on brachial artery.
11. Inflate cuff higher by 20mmHg than the estimated systolic pressure. There should be no sound.
12. Deflate 2 to 3 mmHg/sec until you hear the first KAKAKA RA KOFF sound. This is the SYSTOLIC PRESSURE. REMEMBER THE PRESSURE
13. Continue to deflate until sound disappears. This is the DYSTOLIC PRESSURE. REMEMBER THE PRESSURE.
14. Deflate completely and remove cuff.
15. Ask patient if he/she has any questions.
16. THANK PATIENT........ and get your butt out of the LS and to the next LS! or if it's your last station, go celebrate!
Sunday, October 18, 2009
LAST PCL... awwwwww... ;(
2. Social relationship- adolescent,puberty - IAN
3. Embryological development - PIKKYnieus sp.
4. Prenatal diagnosis, prevention - folic acid (dosage) - PHEY CHIEN CHIEN
5. Medical issues - incontinence - bladder and bowel, lack of sensation, gait, VP shunt complications(blockage?). Dermatome map - BITCH WHORE SLUT, DINNY
6. Management of urinary incontinence - RUN RAN RUN
7. Sore- foot infection, treatment, consequences, implications if not heal (necrosis) - WAI KITTY
9. Hydrocephalus - BERT-RAND
10. Educational issues- Jeevithaaaaaa
Saturday, October 17, 2009
Clinical Skills Revision Practice!
18 more dayssssssssssssssss...........................
Friday, October 16, 2009
Cultural Issues involving doctor patient communication
Transport: Challenges here include availability of private or public transport, including drivers, as Goori women often do not have a license, and conditions of the road, especially in our flood prone areas.
Finances: This features in every detail from telephone or radio access, to payment for transport and medical services.
Social Supports: Childcare is especially important in these communities, as the cost and ability to take the whole family along is often impossible. Cultural or family responsibilities are often obligations greater than the individual need.
Disability: A further possible limitation, not provided for at many levels.
Cultural appropriateness: An often cited cause for hesitation, including the degree of indigenous involvement in the facility, how aware and how trusted the health practitioners are, and of course language and gender issues, kinship obligations, education.
Timing: All of the above have to then coordinate with service availability and an understanding of appointment systems.
Paperwork: Attainment of appropriate identification such as Medicare card, Healthcare card or license, are made especially difficult if they have no birth certificate or are unable to fill in the paperwork due to illiteracy.
Fear: Fear of big buildings, especially when having to go up flights of stairs away from the earth’s force; fear of hustle and bustle and confusion; fear of judgment; fear of misunderstanding; fear of pain; fear of poor prognosis; fear of death; fear of embarrassment or having to discuss private or taboo subjects; and basic fear of western culture including medicines or invasive treatments.
Thursday, October 15, 2009
life in sarawak
Ibans were called Sea Dayaks.
The Ibans were unfortunately branded for being pioneers of headhunting. Headhunting among the Ibans is believed to have started when the lands occupied by the Ibans became over-populated.
The Ibans were traditionally animist, although the majority are now Christian, some of them Muslim and many continue to observe both Christian and traditional ceremonies, particularly during marriages or festivals.
Significant festivals include the rice harvesting festival Gawai Dayak, the main festival for the Ibans.Other festivals include the bird festival Gawai Burong and the spirit festival Gawai Antu. The Gawai Dayak festival is celebrated every year on the 1st of June, at the end of the harvest season, to worship the Lord Sempulang Gana. On this day, the Ibans get together to celebrate, often visiting each other. The Iban traditional dance, the ngajat, is performed accompanied by the taboh and gendang, the Ibans' traditional music. Pua Kumbu, the Iban traditional cloth, is used to decorate houses. Tuak, which is originally made of rice, is a wine used to serve guests. Nowadays, there are various kinds of tuak, made with rice alternatives such as sugar cane, ginger and corn.
The Gawai Burong (the bird festival) is held in honour of the War God, Singalang Burong. The name Singalang Burong literally means "Singalang the Bird". This festival is initiated by a notable individual from time to time and hosted by individual longhouses. The Gawai Burong originally honoured warriors, but during more peaceful times evolved into a healing ceremony. The recitation of pantun (traditional chants by poets) is a particularly important aspect of the festival.
For the majority of Ibans who are Christians, some Chrisitian festivals such as Christmas, Good Friday, Easter, and other Christian festivals are also celebrated. Most Ibans are devout Christians and follow the Christian faith strictly.
The Iban as well as the Kayan also play an instrument resembling the flute called 'Sapek'. The Sapek is the official musical instrument for the Malaysian state of Sarawak.
HEALTHCARE IN SARAWAK
* Sarawak has 194 rural health clinics that function as "one-stop" family health centres
* provide an integrated service comprising
o maternal & child care
o general outpatient care
o environmental sanitation
* All clinics have rest beds and birthing facilities to encourage safe delivery among rural mothers* Community clinics are smaller versions of health centres and serve between 1,500 - 3,000 people.
* Except for a few larger clinics with medical officers, all rural health facilities are managed by allied health personnel
HEALTH SERVICE DELIVERY SYSTEM
Hospitals
- 3 types of hospitals in the Sarawak
- The district hospitals without specialists , managed by medical officers.
district hospitals with specialists (previously known as divisional hospitals)
- The Sarawak General Hospital in Kuching
Polyclinics
- These are large urban clinics managed by medical officers.
- provide:
:general out-patient care,
:maternal and child care
:dental care.
:laboratory and
:radiological services.
Mobile Health Services
- in the form of Village Health Teams and Flying Doctor Service, to serve people in less accessible areas.
- These teams either travel by road, river, on foot or by helicopter, depending on the accessibility of the areas they serve.
Flying Doctor Service
- introduced in 1973
- provide basic health services to people living in remote areas.
- The service operates 3 helicopters that are rented under a contract with a private company.
- The helicopters are based in Kuching, Sibu and Miri and together, they cover 175 locations throughout the State with a population of about 70,000.
- The Flying Doctor team comprises a medical officer, a medical assistant and two community nurses
- visit tp locations once a month or once in two months.
Village Health Promoter Programme
- provide basic health care to these communities on a more continual basis.
- two volunteers from each participating village are given three weeks' training on a fairly wide-range of health-related topics.
- these volunteers give first aid,do health promotion, make blood slides for detection of malaria parasites and sputum slides for detection of tuberculosis,
give regular feedback on their activities
- regularly supervised by staff from the Sarawak Health Department.
- From 1981 -2001, there were 2,956 VHP throughout the State, serving a total of 271,182 people from 1,664 villages.
"Home-based" Health Records
- was introduced in the 1970's for the child-health card,
- the 1980's for the antenatal card and
- in 1992, for the outpatient card.
- it ensures continuity of care for the patient, especially in children, where immunisation records are concerned.
REFERENCE
http://www.sarawak.health.gov.my/about.htm
Impact of Diabetes on Wound Healing
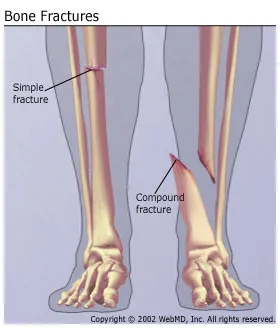
Types of fractures
Open or compound fracture. The skin may be pierced by the bone or by a blow that breaks the skin at the time of the fracture. The bone may or may not be visible in the wound.
Transverse fracture. The fracture is at right angles to the long axis of the bone.
Greenstick fracture. Fracture on one side of the bone, causing a bend on the other side of the bone.
Comminuted fracture. A fracture that results in three or more bone fragments.
spiral - the break spirals around the bone; common in a twisting injury
oblique - diagonal break across the bone
compression - the bone is crushed, causing the broken bone to be wider or flatter in appearance






Wednesday, October 14, 2009
complications of compound fractures
Gas gangrene :
-soft tissue necrosis provide a good anaerobic breeding ground for the clostridial organisms
*May impair the circulation and make the infection more severe
-produce exotoxins which cause Toxemia, depression, perpheral circulatory failure
-The proteolytic organisms break down the muscle proteins and liberate hydrogen sulphide and ammonia gases
*responsible for the bad smell.
Tetanus :
- increased muscle tone and spasms
* caused by the release of the neurotoxin tetanospasmin by Clostridium tetani
-Should be prevented with anti Human tetanus immunoglobulin or antitetanus serum.
Crush Syndrome :
-ischemia of several hours is relieved suddenly
-the products of muscle breakdown (myohemoglobin) enter the general circulation.
* large quantities of potassium, phosphate, myoglobin, creatine kinase and urate
-renal tubular obstruction and renal damage
Late Complications :
Chronic osteomyelitis
-inflammation of the bone
-staphylococcus aureus
-discharging pus and forming a sinus
-discharge of the sequestrum.
Skin loss with thin and adherent skin
Non union with bone segment loss.
Surgical Management of Open Fracture
Grade I: Small skin laceration by tip of spiral fracture
Grade II: Small to moderate, well circumscribed wound. No significant tissue necrosis
Grade IIIA: Longer laceration with significant contused or non-viable tissue. After debridement, delayed suture of split thickness skin graft (STSG) can close wound.
Grade IIIB: Extensive soft tissue wound with crush. Local or free muscle flap required.
Grade IIIC: An open fracture with vascular injury that requires vacular repair to salvage the limb.
Grade IV: Total or subtotal amputation
Pre-operative
Take history
Physical Examination
Complete blood test
Radiographs- anteroposterior and lateral radiographs of the injured leg.
The ipsilateral knee and ankle are also often radiographically imaged. Why?
A CT scan and an MRI may be obtained.
Radical debridement of necrotic tissue, and prophylactic intravenous antibiotics.
Intra-operative
The procedure involves using a large surgical incision, reducing the fracture, placing a metal plate over the fracture, and fixing the plate onto the bone with multiple screws.
Because of the extensive soft-tissue manipulation required, plating can be difficult for the surgeon and damaging to the local vascular supply.
External fixation is a widely used and very successful method for treating some types of tibial shaft fractures.
The procedure involves multiple pins attached to the external rods to maintain length and alignment.
Post-operative & follow-up
Long-term outcomes for tibial shaft fractures generally are good, but a small increase in osteoarthritis of unclear etiology in the knee and ankle has been observed
After surgery, the patient should be monitored in the post-anesthesia care unit until stable.
Depending on the extent of the other injuries, the patient may be transferred to the surgical intensive care unit or to a regular ward bed.
Initially, the patient's vital signs should be monitored repeatedly, with careful attention paid to any abnormalities.
If a complication occurs, early discovery almost always improves the prognosis.
On the first postoperative day, the patient should be examined by the surgical team and a complete blood count should be obtained.
Once the patient has recovered from surgery and is considered safe to leave the hospital, he or she should be discharged to home or to a suitable rehabilitation facility
Prevent wound infection+Tetanus

Tetanus Prevention
1. Prevent tetanus through immunization -- An effective vaccine against tetanus has been available for many years. It is usually given to children combined with diphtheria and pertussis vaccines in a shot called DTP. A child needs five DTP shots, given at specified intervals, for complete protection. Tetanus booster shots are recommended every 10 years. Persons with wounds that are deep or dirty may need a tetanus booster shot if more than 5 years have passed since the last dose. An injection of tetanus immune globulin (TIG) given as soon as possible after a tetanus-prone injury can also help neutralize the poison that has not entered the nervous system.**
2. Prevent tetanus through proper care of wounds -- Cleaning all wounds, removing dead tissue, and using antibiotics for contaminated or infected wounds can reduce the likelihood of getting tetanus.
** Immunization in Malaysia (Refer to table above)
If you have never received a primary immunization as a child and you have an open wound, the doctor will likely give you the first vaccine dose at the time of your wound care, as well as a single dose of a special immunoglobulin with high activity against tetanus. You must see a doctor in four weeks and again in six months to complete the primary vaccination series.
Prevent wound infection
1. Wash your residual limb with mild soap and water, then rinse and pat dry. Do this at least once a day; do it more often if you sweat a lot or are treating a rash or infection.
2. Wash anything that comes into contact with your skin (liners, socks, inner socket, etc.) with mild soap and water, then rinse and dry.
3. Do not use alcohol-based lotions on your skin. They cause the skin to dry and crack, increasing the chance of infection.
4. Do not use too much softening lotion; use just enough to prevent dry skin.
5. Maintain a good prosthetic fit at all times and take care to maintain correct alignment and socket fit. Having the right fit will help relieve pressure spots and soreness.
6. Eat a balanced diet and drink plenty of water to maintain supple, healthy skin.
7. If you are a diabetic, monitor and maintain your glucose levels.
Symptoms of bacterial infection, immediately go seek doctor for further treatment:
- area around the wound feels hot
- area becomes red and swollen
- pus or white/yellow drainage
- sudden increase in pain
- severe tenderness
- fever
Sunday, October 11, 2009
PCL Week 12 Tasks
1. Life in Sarawak (Jeevitha)
2. Anatomy of calf muscle (Bert,Matt)
3. Complication of fractures (Phey Chien)
4. Types of fracture (Pik Yin)
5. Surgical management of fractures (Ian)
6. Cultural issues in treating indigenous people(Wai Kit)
7. Healthcare assist in supporting them(Niva)
8. Prevent infections & how to prevent tetanus ( Dean)
9. Impact of diabetes on wound healing (Mitch)
10. Compartment syndrome (Ran)
Saturday, October 10, 2009
OSCE practice session
we got a clinical skills practice session for our formative OSCE on MONDAY 10-11am..its just before PCL, after our morn lecture...
We're gonna be practising on the 2 stations that's coming out this friday yea...so do come...its COMPULSORY...1 hr of practice only k...if we need more we can do it on tues or another day k =)
Thanks!!
Thursday, October 8, 2009
Carpo pedal syndrome
A spasm of the feet and hand observed in hyperventilation, calcium deprivation, tetany.
-Associated with tetany
-Lowered muscular excitability threshold
-Results in involuntary spasms
-Diffuse muscles involved in severe, spontaneous tetany
-Laryngeal Stridor (noisy breathing, crow like)
-Generalized Tonic Clonic Seizure (seizure involving the entire body. It is also called a grand mal seizure. Such seizures usually involve muscle rigidity, violent muscle contractions, and loss of consciousness)
-Death may occur
Causes
-Hyperventilation
-Hypoparathyroidism
-Hypocalcemia
-Hypomagnesemia
Pathophysiology of hyperventilation
-Triggered by fear, anxiety, stress or pain.
-Involves increasingly rapid breathing.
-Respiratory rate ↑, CO2 level ↓ resulting in alkalosis.
-Causes left shift of oxyhemoglobin disassociation curve in which the hemoglobin hold on tightly to O2 and does not unload them effectively.
-Results in hypoxia and anxiety.
-Carpopedal spasm is a characteristic sign of respiratory alkolosis.
-Involves tingling and contraction of hands and feet due to hypocapnia (↓ level of CO2).
Indications of carpopedal spasm
Trousseau’s sign
-Technique
Occlusion of brachial artery with BP cuff for 3 minutes
-Interpretation: Positive test suggests Carpopedal Spasm Carpal Spasm symptoms elicited
Chvostek’s sign
-A sign of tetany seen in hypocalcemia.
-Tap facial nerve at the angle of jaw (masseter muscle) , facial muscles on the same side will contract momentarily.
-This is due to hypocalcaemia, with hyperexcitability of the nerves
Signs and non surgical treatment for ACL tear
- Hearing a ‘pop’ sound
- Knee giving out- unstable
- Swelling associated with hemarthrosis and pain
- Unrepaired ACL tears may also lead to early arthritis in the affected knee.
Non surgical treatment
-Decrease pain and swelling in knee by giving simple analgesics eg: acetaminophen or NSAID
-Rest
-Use crutches until you can walk without a limp
-Placing a needle in the swollen joint and aspirating (or draining as much fluid as possible) gives
relief from the swelling
-Physical therapy such as ice, electrical stimulation, and rest periods with your leg
supported in elevation
-Exercises are used to help you regain normal movement of joints and muscles. Exercise helps improve the strength of the hamstring and quadriceps muscles
- ACL brace. usually custom-made
Wednesday, October 7, 2009
Knee Joint examintaion
- The patient's foot is wedged between the examiner's body and elbow.
- The examiner places one hand flat under the tibia pushing it forward with the knee in extension.
- The other hand is placed against the patient's thigh pushing it the other way.
- The lower limb is taken into slight abduction by the examiner's elbow with the examiner's body acting as a fulcrum to produce the valgus.
- Th examiner maintains the anterior tibial translation and the valgus and initiates flexion of the patient's knee.
- At about 20-30 degree, the pivot shift will occur as the lateral tibial plateau reduces
- It is positive when the proximal head of a patient's tibia can be pushed posteriorly on the femur.
- The patient is placed in a supine position and the knee is flexed to approximately 90 degree with the foot in the neutral position.
- The examiner sits gently on the patient's foot placing both thumbs on the tibial tuberosity and pushing the tibia backward.
- If the tibia plateau moves, the posterior cruciate ligament is torn.
Knee examination
Rather good website found in the knee joint practical.
Tuesday, October 6, 2009
Physical examination of the knee - Lachman's test and anterior drawer test.
Tests for: Anterior cruicate ligament
Look for: End point of the ligament
Points:
- Patient lies down on his/her back
- Slightly flex the knee about 20-30 degrees to relax quadriceps and hamstrings
- Support distal femur
- One hand on the tibial tubeosity/proximal tibia
- Apply a force anteriorly on the tibia.
- If it doesn't come to a stop, ACL tear.
Tests for: ACL
Look for: More than 5 degrees of movement of the tibia anteriorly
Points:
- Patient lies on back
- Knee flexed to 90 degrees
- Ensure hamstrings are relaxed
- Examiner sits on the foot
- Pulls the tibia anteriorly
- According to Gray's, the medial meniscus or meniscotibial ligaments MUST be damaged to elicit this sign.
Others
- Look for varus and valgus when checking posture
- Test range of movement/tone, power, bulk.
- Patellar tap - bulge sign
- Patellar apprehension test
- Apley's grinding test - meniscal damage
- Distraction test - meniscal damage
- Baker's cyst
- McMurray's test - meniscal damage
Knee Joint Task Allocation
(Use articulated skeletons & bone sets, models, plastinated specimens & prosection photos)
Wai Kit
1.1. Review the features in the articulating surfaces of the knee joint:
1.1.1. Distal Femur:
1.1.1.1. Lateral and medial condyles and intercondylar fossa
1.1.2. Proximal tibia
1.1.2.1. Lateral and medial tibial plateau
1.1.2.2. Intercondylar tubercles
1.1.2.3. Intercondylar eminence
1.1.2.4. Lateral & medial condyles of tibia
1.1.2.5. Anterolateral ( Gerdy) tubercle
1.1.2.6. Tibial tuberosity
Niva
1.2. Identify the patella
1.2.1. Identify its apex and margins
1.2.2. Identify the medial and lateral areas and its subdivisions in its posterior articular surface
1.2.2.1. In which movements does these different facets come in contact with the femur?
1.2.2.2. Why is patellar movements examined in full extension?
Matt
1.2.3. What types of bone is it?
1.2.3.1. How does this explain the fact that when it fractures, bony union does not take place easily
1.2.4. In what clinical condition does it simulate a fracture?
Pikky
1.3. Why does patella have a natural tendency to displace laterally?
1.4. What normally prevents a lateral patellar displacement?
2. Activity 2 : Muscles, Fascia & Ligaments
(Use articulated skeletons & bone sets, models, plastinated specimens & prosection photos)
Jeevi
2.1. List & identify the muscles that flex and extend the knee joint.
2.2. Identify the collateral ligaments
2.2.1. How are they different in shape and attachments from each other?
2.2.2. Which structure runs deep to each collateral lig.?
2.2.3. What is found between the lateral ligament & meniscus?
2.3. Explain why a tear of Medial Collateral ligament is associated with medial meniscus tear
2.4. What structures crosses the MCL?
2.4.1. What intervenes between these structures?
2.5. How will you test the stability of the collateral ligaments?
Ian
2.6. Identify the patella tendon.
2.6.1. What are its attachments?
2.6.1.1. What are the clinical applications of this?
2.6.2. When the knee joint is locked which is the only ligament which is not taut?
2.7. Draw a schematic diagram to show the following features and attachments of the upper surface of the tibia: Attachments of the medial and lateral menisci, ACL PCL Shapes of medial and lateral meniscus Transverse ligaments Tibial Spines
PC
2.8. How does the medial meniscus differ from the lateral in shape, attachments and functions?
2.9. Enumerate the functions of the menisci
2.10. What are the different types of Meniscal tears?
Mitch
2.11. Identify the ACL and PCL
2.12. Identify their attachments
2.13. What are the functions?
2.14. What are the components of O‟Donahue‟s Triad/ Terrible Triad?
2.14.1. Demonstrate the mechanism of injury
http://rad.usuhs.edu/medpix/medpix.html?mode=case_viewer&imid=18313&pt_id=6681&quiz=&th=&table=card&showall=#pic
3. Activity 3 : Joints
(Use articulated skeletons & bone sets, models, plastinated specimens & prosection photos)
Ran
3.1. Functionally knee joint is a modified hinge joint – Explain how in relation to shifting of its axes of movement
3.1.1. Briefly discuss the key factors that contribute to the stability of the knee joint.
3.2. Identify the knee joint line
3.2.1. What is the normal “Q” angle of the knee joint ?
3.2.1.1. How does it differ between sexes?
3.3. What obstetric history is present in a person with “ genu recurvatum”?
3.3.1. What is “genu valgum” and “genu varum”?
3.3.1.1. How does these conditions predispose to the degenerative changes in the knee?
Dean
3.4. Demonstrate and explain on an articulated knee, the locking and unlocking of the knee joint.
3.4.1. Which muscle is involved in unlocking?
3.5. Identify the clinically important bursae around the knee joint.
3.5.1. Which of these communicates with the knee joint?
3.5.1.1. How is this clinically important?
3.5.2. What is „Housemaid‟s knee‟?
3.5.3. What is „Clergyman‟s knee‟?
4. Activity 4 : Surface Anatomy
http://www.sportsdoc.umn.edu/Clinical_Folder/Knee_Folder/Knee_Exam/lachmans.htm
Bert
4.1. How will you test for Anterior/Posterior Instability of the Knee joint?
4.2. Demonstrate the Anterior and Posterior drawer signs and the Lachman‟s test.
5. Activity 5 : Procedural Anatomy
5.1. Where will you do an aspiration of the knee?
6. Activity 6 : Radiology
{Refer to radiological images in textbooks & Clinical Imaging software Radiology 2; http://www.radiologyassistant.nl/en/42764e8fe927e }
6.1. Study the following :
6.2. Review of X-ray of the Knee joint (AP & lateral views)
6.3. MRI of the Knee joint : Coronal and Axial images
Task allocation :
1. Wai Kit
2. Niva
3. Matt
4. Pikky
5. Jeevi
6. Ian
7. PC
8. Mitch
9. Ran
10. Dean
11. Bert